In September 2013, the Halle Saint Pierre gallery in Montmartre mounted an exhibition celebrating the 25th anniversary of the British magazine Raw Vision. The magazine, like the gallery, is devoted to Art Brut, a movement that insists on the value of art made by self-taught artists, including patients in psychiatric hospitals. I visited the exhibition by accident, wandering in during a weekend in Paris, and found pictures of tree roots made up of twisted and tortured bodies; of Adam and Eve stripped of their skin, so that they looked like illustrations in a medical dictionary or a butcher’s diagram; of a man with a fish for a penis; of exploded heads; of bodies trapped in machines. I turned from these scenes to a set of images that appeared less frightening: pictures of strange birds, mammals and fish drawn crudely on small rectangles of paper by an artist known as J.J. Beegan, who was a patient in an English asylum in the 1940s.
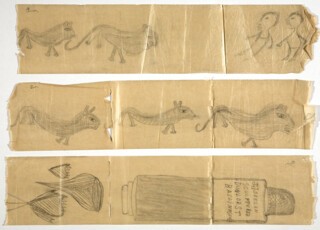
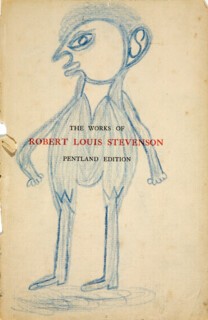
Most of the drawings were done painstakingly with rudimentary materials: the char from burned matches on Izal medicated toilet paper – the hard, shiny paper that was common in British institutions throughout the 20th century. These images were of curious creatures with human-like mouths, and of human figures with faces in profile. Another drawing was done with a nurse’s blue pencil on the flyleaf of a volume of The Works of Robert Louis Stevenson.
‘These drawings were presented to me by a very ill man,’ the catalogue entry read, quoting Edward Adamson, the art therapist who first encountered J.J. Beegan in 1946. By the time they met, Adamson explained, Beegan ‘had been in a locked ward in the hospital for many years. He was incontinent and unable to speak clearly. He drew vigorously on the only paper he could find.’ Adamson, who was tasked with introducing art therapy to the hospital, brought Beegan to his studio and gave him an easel, large sheets of paper and materials to work with. Beegan took to filling the paper with drawings of men and animals, and writing out abstruse, disconnected thoughts, or maybe messages. ‘This man lived in a world of his own. He did many similar drawings, covered with esoteric writing which obviously had a private meaning for him.’
I was struck by the naive pictures, but more so by the fact that Beegan had been a patient at Netherne Hospital in Coulsdon, where, in effect, I grew up. This is a slight exaggeration: Netherne was where my mother worked, and my grandparents worked before that, and where I spent a great deal of time when I was young.
It was strange, being able to imagine the rooms in which Beegan had lived – or, more accurately, since I never went into a locked ward when I was a child, the corridors he walked to get from the ward to the art studio and back. I remembered those corridors well, and I remembered how much I disliked them. The shiny, dun-coloured institutional paint; the double fire doors with plastic portholes; the windows that were a bit too high to see out of – at least for me. I wondered what it had been like behind the locked doors. I wondered what kind of matches would give you enough charcoal to make a small drawing, and how Beegan got hold of them.
When I returned to London I looked up Edward Adamson, and the collection of artworks he built during his 35 years at Netherne. This led me, some months later, to an office in Lambeth belonging to David O’Flynn, a consultant psychiatrist at the Lambeth and Maudsley Hospitals, and chair of the Adamson Collection Trust. We walked up and down the corridors of the clinic where he worked and looked at the display of patients’ pictures on the walls (these were copies of the originals, which are held in the Wellcome Library archives at Euston). We talked about the images, and the different uses to which they have been put. Until the 1950s, art done in psychiatric hospitals tended to be used as a diagnostic tool. Doctors and therapists would attempt to ‘read’ symptoms, such as dissociations and phobias, from paintings and drawings; some hospitals keen to try out new treatments experimented with getting patients to produce ‘before’ and ‘after’ paintings, to see if they could identify any improvement. But Beegan did his drawings on his own.
Soon after his arrival at Netherne in 1946, Adamson explains in his memoir, he visited the locked ‘back’ wards of the hospital:
Having passed through long corridors and many locked and relocked doors, I was ushered into a large hall containing about a hundred people … Many of the inhabitants underwent major brain operations, and consequently many were shaven-headed. Others were swathed in bandages and were disfigured by post-operative bruises and black eyes.
The patients were dressed in hospital-issue clothing and had no personal possessions. I wondered where Beegan kept his pictures. Under a mattress? Inside The Works of Robert Louis Stevenson? Or did he carry them on his person at all times? There is no record of the illness that afflicted him, or of the treatments he received. We know only that he was kept in the locked ward with other bruised and battered men for many years. It is likely that he had had his teeth removed, and possibly other organs too, following the ‘sepsis’ theory of mental illness that was popular in the 1920s, or that he underwent brain surgery, or insulin coma therapy, or electroconvulsive therapy, or all three. He may have had seizures induced by injections of cardiazol. All these therapies were common in the hospital through the 1930s and 1940s, for illnesses as diverse as schizophrenia and epilepsy.
In the film Abandoned Goods (directed by Edward Lawrenson and Pia Borg), which traces the history of the Adamson Collection, the curator of the Halle Saint Pierre, Martine Lusardy, describes what it feels like to handle these drawings:
The material is so precarious, fragile. There is a kind of humour in it. It’s toilet paper … It’s the most prosaic, vulgar material … but suddenly you forget what it is and it becomes a parchment, a precious object … The way they are looked at has changed. It’s no longer a clinical gaze, but [an] aesthetic and artistic one. The work has changed status, which changes the status and identity of the people who created it. They are given back their place among human beings.
I liked the sentiment but wasn’t sure I believed it. It would be nice to think that focusing on the aesthetic qualities of Beegan’s drawings – rather than trying to diagnose him – would take us closer to the man himself. But I am not convinced that that is what Art Brut does for Beegan. It’s hard to get past the toilet paper, and the strange romance of a man in the bleakest of circumstances continuing to make images. I read recently of a man kept in solitary confinement in a Californian prison for twenty years, who painted with the pigment from M&Ms and Skittles (dissolved in a little water) and a paintbrush made with strands of his own hair wrapped around the barrel of a plastic prison-issue pen. He described ‘the ritual aspect of cleaning the work area, mixing the colours, doing the base, and laying out the brushes and water in milk cartons or rinsing and getting started’, and I wondered if this came close to the kind of freedom in concentration that Beegan may have found as he rubbed and scored with burned matches. What I was looking for was permission to believe that Beegan was indeed able to exist ‘in a world of his own’, his esoteric writings a sign of his secret life, not completely dimmed by the circumstances of his incarceration. I’m not suggesting we shouldn’t look in hope for the places where creative survival might be found. It’s just that I doubt this gets us closer to the man himself.
Some of the writing on the drawings is, as Adamson put it, esoteric. One drawing, done in the art studio on a large sheet of paper (and with a pencil), includes the following set of words, which I couldn’t help thinking may have been partly inspired by Stevenson. For how long had that book been his only companion?
Wait [near/new] M page cue
M qu [enos] sedge country brid low [people ago dons] biaz
be Queer oranges VIATI false teethrillrer newtos winter autumn dies when
we are him
memo septuesguesim ALSORT Joel boy [eos/is] Galleon eh
Treasure Isles
But some of the writing is extremely clear. There are two similar drawings done with charred matchsticks on toilet paper, which he must have executed in the locked ward before he met Adamson. One is of something like a medicine bottle, with a label that reads:
JJ BEEGAN
SCULPTURER
DUNLOR ST
BALLINASLOE
The other is of one of his characteristic flattened faces in profile, sitting on top of a triangular body, like a cone, drawn in such a way as to suggest three dimensions. Both the bottle and the triangular figure feature the same ‘stand’ drawn underneath them – it’s this that helps give them their three-dimensional appearance, and marks them out as works of art, as though they are drawings for stand-alone sculptures. Underneath the man-cone he has marked the words:
JJ BEEGAN
SCULPTURER
DUNLOP HILL
BALLINASLOE
The voice narrating the film David and I watched that day on his NHS computer sounded familiar. I couldn’t put my finger on it, but it turned out to be the writer Iain Sinclair. When we got to the bit in the film where Sinclair describes these images and reads out the script, I asked David to pause it for a moment. ‘It’s Ballinasloe,’ I said, ‘with the accent on the last syllable. Not Ballinasloe, with the accent in the middle.’ Ballinasloe is a town in Galway, famous as the site of one of the largest mental asylums in Ireland. I was struck by the fact that the name didn’t ring any bells with David – after all, he was a psychiatrist, and interested in the history of his field. But I caught hold of myself. Why should it be a surprise that the Ballinasloe asylum – now known as St Brigid’s Hospital – is famous only in Ireland? Lots of things that are famous in Ireland are only famous there.
But the voiceover grated a bit. Perhaps it was just the fact that Sinclair didn’t know how to pronounce Ballinasloe, but it felt to me as though he, or the directors of the film, liked words that didn’t make sense. The esoteric writing, and its private meanings, suited them. It struck me that the clinical and aesthetic responses to the work were not as far apart as they seemed. They were both heavily invested in the idea of a secret significance. But it looked to me as though Beegan was writing down his name and address. With all this interest in the drawings, I wondered why nobody had looked him up.
When I got home that evening I searched online for Dunlop Hill in Ballinasloe. ‘Dunlop hill is a hill in Dunlop, East Ayrshire,’ Google told me, but it also asked: ‘Did you mean: Dunlo Hill Ballinasloe?’ And I did, or rather J.J. Beegan did. When I turned to the Irish census records I could quite easily find John Beegan, who was born in 1868, the eldest child of John and Jane Beegan. In 1901 they were living together with the younger Beegans, Mary and Thomas, at 23 Dunlo Hill in Ballinasloe. On the census form, John Beegan senior describes himself and his two sons, John Leo and Thomas, as stonecutters. Ten years later, in the 1911 census, he chose the term ‘monumental stonemason’ – the family were skilled craftsmen, who worked primarily cutting and carving gravestones. They did high-class, ornate work and had a good reputation; some of the early 20th-century memorials at Kilbegley graveyard in nearby County Roscommon are signed by the Beegan stonemasons. There is a large Celtic cross carved by them as a memorial to the 4th earl of Clancarty, and erected over his grave at Highgate Cemetery, just up the road from where I now live.
By the time of the 1911 census John Beegan’s eldest son, John Leo Beegan, was married, and living in another, slightly grander house on Dunlo Hill – a double-fronted town house, with its own stables, a piggery, a hen house and other outbuildings. He lists his profession as ‘sculptor’. I could discover, too, that he had married Mary Anne Beirne two years earlier, and that they now had a baby son, also called John. Mary Anne was the eldest daughter of the local butcher, who was the Beegans’ neighbour on Dunlo Hill. Beegan married up; the Beirne family could afford to have three servants living with them. The wedding was held in Rathmines, a middle-class suburb of Dublin. Either they had money and connections, or at least one set of parents disapproved of the marriage and they eloped, to return home with the union accomplished.
I could keep going. I could tell you about the struggle in the late 19th century between skilled artisans and local farmers in Ballinasloe, about the land the Beegans rented in the quarry for their stone, about the huge stone that lay outside the Beegans’ home on Dunlo Hill for more than fifty years, waiting to be carved into a memorial for the Battle of Aughrim, about John Leo’s debts, and his run-ins with the owner of the local newspaper, William Hastings. All this and more can be discerned from census returns, court records and newspaper archives. And I imagined things that I couldn’t actually prove. I wondered if, when he was in Dublin (to get married, for example, or to help transport the Clancarty memorial to London), John Leo Beegan met another stonecutter about his own age, Willie Pearse. Willie and his older brother, Patrick, both of whom were executed for their part in the Easter Rising, were the sons of a monumental stonemason. Pearse’s ecclesiastical architecture and stonemasonry business was on Great Brunswick Street in the centre of Dublin, round the back of Trinity College. But to tunnel in that direction (political history, famous men) was to find shelter inside a more familiar historical narrative. I was looking for evidence of something else.
Ispent months inside the world of the Beegans of Ballinasloe, or as far inside as I could get, reading local histories, studies of the politics of the nearby landed estate, books about ecclesiastical architecture and histories of Ballinasloe asylum. I made contact with genealogists, local historians and eventually even surviving members of the family. During lockdown in the spring of 2020 I used my government-sanctioned hour of exercise to circle the perimeter of Highgate Cemetery, to see if I could spy the Beegan memorial from afar. All the time I was hoping to turn up a clue to the precise identity of the man at Netherne. I knew that he wasn’t any of the obvious John Beegans of Dunlo Hill – the ones I could find in the census – because they all died at home in Ballinasloe, not in an English mental hospital. For a while I became fixated on a missing death registration. John Leo Beegan died of pneumonia in February 1922, in his early fifties, but his death wasn’t registered until 1935, when the Widows’ Pension Act was passed. I wondered whether John Leo (who, after all, lived on Dunlo Hill and described himself as a ‘sculptor’ in the 1911 census) had got himself into some sort of trouble and absconded. It was the period of the civil war in Ireland, when social bonds were often stretched to breaking. I plotted a story that took him by way of Dublin to London and more trouble. I had a theory about drink and delirium, which got him committed to Netherne asylum, and a long incarceration. I was quite convinced by it until I discovered a newspaper report of John Leo’s funeral in February 1922. Whoever J.J. Beegan of Netherne was, it wasn’t him.
But I really wanted to find him. If we were to give Beegan back his place among human beings, I reasoned, we needed to know who he was. But I didn’t find J.J. Beegan. All I found were a number of leads that didn’t quite take me where I wanted to go. There was a record of a birth in Ballinasloe Workhouse, in 1915, of a child called John Beegan. His mother, Annie, was unmarried. She seems to have returned home at some point to a farm near Ballinasloe, where she lived until she died, still single, in the 1960s. But what happened to her child? I could find no record of his death in Ireland, but that may be because he died young. The deaths of children who died in infancy (particularly if illegitimate and born in the workhouse) were often not recorded. But if this child survived, was he taken in by his relatives, the Beegans of Dunlo Hill, and did he work for them? Did he set out on his own as a teenager or young man, and did he end up out of work in London? I imagined him as a young man in England: a west of Ireland accent; little preparation for city life. At some point he was picked up by the police and locked away. Was he homeless? Was he violent? At this point there was very little difference between my attempts to find out more about J.J. Beegan and storytelling.
And I could see that my obsession with finding the man behind the drawings was out of kilter with the material – the doodles on loo paper. I went back to the pictures to see what story they told. The drawings are of human figures, birds and animals. On a drawing of two fish he wrote: ‘BULLFISH SIMLER TA PERCH FOUND IN TH RIVER BARROW’, and ‘FIKE [Pike] N AUGHRIM RIVER’. The rivers Barrow and Aughrim are in the south-east of Ireland, in Wexford and Wicklow. So perhaps the pictures tell us simply that Beegan liked fishing – the mouth of the bullfish is drawn with exquisite attention – and that he travelled to some of the best fishing spots in Ireland. But I think that what the drawings say above all is that this was a man who remembered. His drawings were not an imaginative flight into another experience, or a representation of his struggle with inner conflict: there are no people stripped of skin, no tortured bodies. The drawings were a way of remembering. They were his connection with the world outside, the world he knew before his life came to a stop and he entered the asylum.
J.J. Beegan was living in his own afterlife. The future was taken away from him and he chose not to live in the present. He didn’t draw the people around him on the ward or the views from the windows; he drew what he remembered from the life he had lived before. His pictures were his only means of communication, including perhaps with himself. On them he kept writing a name and address – the person he thought he should have been, or perhaps the person he wished he had been: J.J. Beegan, Sculpturer, Dunlo Hill, Ballinasloe.
Netherne’s case records are closed, so I can’t find out when J.J. Beegan entered the hospital, or why. But a friend suggested I try the 1939 register – a register of the wartime population of Britain that included hospitals and prisons. It would at least give me a birth date. The register is easy to access online. There are nearly a thousand names on the list compiled at Netherne, each patient listed by surname, forename, date of birth and sex. The list is organised by ward rather than alphabetically, so it took some time to check through. And what I discovered was that the name Beegan doesn’t appear at all. This was at least confirmation of something I suspected but didn’t want to acknowledge: that J.J. Beegan was probably someone else entirely – someone who knew Ballinasloe and knew the Beegans, because he knew where they lived. Perhaps a labourer who worked for them for a while, cutting stone, or a neighbour. This was a disappointing discovery, mainly because it meant there is very little chance of ever working out who the artist known as J.J. Beegan really was.
But as I looked at the long, carefully inscribed list of names I was bothered by something else. The handwriting was extremely familiar. The list appeared to have been written by my father. My father’s handwriting is neat, and even. When I was small I was always in trouble for my blotchy attempts at cursive script. I could never get the nib at the right angle and I dripped ink from the inkwell all over the place: hands, face, clothes and the bits of the paper that were supposed to remain ink-free. I couldn’t draw either. Each evening, when I was five or six, I had to draw a picture representing the story we had heard that day at school and fit it inside a quarter page of my homework book. The twelve labours of Hercules; the loaves and the fishes; the three wise men; Jason and the Argonauts. I was utterly perplexed by the repeated requests to turn a story, with all its twists and turns of events and feelings, into something you could see in a square marked out in pencil on a page. My father took pity and often did the drawing for me, and wrote the caption underneath. I still have that little homework book, and the resemblance between my father’s handwriting and the Netherne register is uncanny.
This was a fantasy, certainly. My father was ten years old in 1939. But when I googled ‘Can handwriting be inherited?’ I read of various experiments measuring the similarity between different aspects of handwriting (orientation, size, letter formation etc). And I learned that the incidence of inherited handwriting characteristics is (or was in these experiments) highest between father and son. It is as high as 98.3 per cent. The register must have been produced by my grandfather. This was eminently possible. My paternal grandparents lived and worked at Netherne from the mid 1920s, and my father was born there. During my father’s infancy my grandfather worked as an asylum attendant, but by the late 1930s he was profoundly deaf (after a surgical intervention to improve his deafness in one ear was carried out – unbelievably – on the wrong ear) and employed as the hospital clerk. It is likely that at some point during J.J. Beegan’s years at Netherne my grandfather turned the key on him. And maybe he did other things too. Perhaps he was kind to him, perhaps he wasn’t.
Recently we took my father, who was turning ninety, to see the house where he was born, a semi-detached cottage built in the 1920s for Netherne employees. It was hard to see past the people carriers and the four-wheel-drives squeezed onto the newly paved forecourts, or past all the architectural improvements (the porches, the decking, the picture windows, the roof extensions), to the narrow country lane of nearly a hundred years ago. But in the gaps between the houses you could see through to the Farthing Downs below. As a child, if I ever thought of my father’s childhood (which wasn’t very often) it was painted in the colours of Betjeman’s poem ‘Croydon’:
Boys together in Coulsdon woodlands,
Bramble-berried and steep,
He and his pals would look for spadgers
Hidden deep.
We learned that poem at primary school and my own childhood was overlaid with its landscape, since I too lived in Coulsdon, and went blackberrying in the woods with my sisters. We had an apple tree in our garden, so I knew that Betjeman was telling the truth when he said: ‘Pear and apple in Croydon gardens/Bud and blossom and fall,/But your Uncle Dick has left his Croydon/Once for all.’ I don’t think that anyone pointed out to us children that this alluded to the fallen of the First World War, and anyway in my understanding Croydon was a place you arrived at, or came back to, rather than disappeared from.
My mother had come to Croydon from the west of Ireland in the late 1940s, and it was there she met my father. They had travelled in the early years of their marriage, and lived in some exotic places, but now they were back and we were all living in Coulsdon. A generation further back, in the early 1920s, my father’s father had moved out from London and his mother from the South Wales valleys, looking for work, and they had met in Coulsdon, just like my parents. Netherne Hospital was one of a string of large psychiatric institutions that hung like beads around the neck of Outer London. They were built out of town, on high ground and farmland, in or about the last quarter of the 19th century, to cater for the increasing numbers of ‘pauper lunatics’ that were the responsibility of county and borough municipalities under the Victorian poor laws. Standing on the rise at Netherne (with nearly one thousand patients in 1922), you could see the Victorian water tower of Cane Hill Hospital to the north (with approximately two thousand patients), and to the east the towers of what was known locally as Caterham Subnormality, full to bursting with more than two thousand mentally disabled inpatients when my teenage grandmother arrived from her South Wales village to work there as a nursing attendant. Further east was the Croydon Borough Mental Hospital (later known as Warlingham Park), a much smaller outfit with just over six hundred beds and, perhaps not unrelatedly, in the mid 1920s the highest ratio of recovery to admissions in England and Wales. There were barely five miles between them all.
My grandparents met at an air force dance. In 1926 they married and lived for a time in rooms in the grounds of Netherne, while they waited for the new cottages to be finished. They moved to their new home in 1928, or early 1929, shortly before my father, their second child, was born. Before the Second World War, the social world of the hospitals must have felt similar to the early 19th-century villages that grew up around large landed estates. A single employer, accommodation on site, a strict hierarchy of employment, ranging from boiler stokers and farmhands at the bottom to doctors and medical superintendents at the top (it wasn’t unusual for hospitals to segregate the dining facilities of nursing and cleaning staff, upstairs-downstairs style, until the 1950s). The hospital was a self-sufficient community. Netherne had its own vegetable and dairy farm (with labour provided by the patients), a bakery, kitchens, laundry, carpentry and light engineering workshops, a printing press, chapel, library, cinema, dance hall, orchestra, choir, sports facilities and amateur dramatic society. No wonder staff married staff, patients married patients, and sometimes staff and patients married each other. Nearby Cane Hill, which also had a private fire station, got its own railway station in 1899, with a covered walkway leading directly to the hospital. It’s now called Coulsdon South, on the commuter line to London Bridge. With their locked wards and their armies of demobbed soldiers employed as attendants to keep the more unruly patients in check, these hospitals in the 1920s and 1930s were something between state villages and prisons. They didn’t change much over the next twenty years. In 1961 the sociologist Erving Goffman described their American counterparts as ‘total institutions’.
In 1949, when my mother arrived at Netherne to be trained in mental nursing, she was taking a similar route to the one Beegan had taken. It is possible he was still alive when she started working there. It is possible that my mother was one of the nurses who brought him from the locked ward to the studio and back again, along those unpleasant corridors. She remembers delivering patients to Adamson in the studio, and the way he would ask what sort of mood they were in. I am almost certain that my mother’s older sister Mary, who had worked at Netherne since the end of the war, would have encountered Beegan. It is highly unlikely, though, that she would have noticed him. He was simply one of hundreds of bruised and bandaged patients living on the back wards, who had to be managed as best they could.
‘Any fool can turn the blind eye,’ Samuel Beckett says in Murphy (1938), a novel set in part in the Bethlem Royal Hospital near Croydon. The hospital had recently transferred to an airy new site in Beckenham when Beckett’s friend Geoffrey Thompson got a job there as a house physician in 1935. Murphy wangles himself a job as an attendant in the asylum, which Beckett renames the Magdalen Mental Mercyseat. Murphy/Beckett was two years younger than my grandfather, who was at the time working as an attendant less than ten miles away.
He would be expected to make beds, carry trays, clean up regular messes, clean up casual messes, read thermometers, write charts, wash the bedridden, give medicine, hound down its effects, warm bedpans, cool fevers, boil gags, sterilise when in doubt, honour and obey the male sister, wait hand, foot and mouth on the doctor when he came, look pleasant.
He would never lose sight of the fact that he was dealing with patients not responsible for what they did or said.
He would never on any account allow himself to be affected by the abuse, no matter how foul and unmerited, that would be poured out upon him. The patients seeing so much of the nurses and so little of the doctor, it was natural that they should regard the former as their persecutors and the latter as their saviour.
He would never on any account be rough with a patient. Restraint and coercion were sometimes unavoidable, but must always be exerted with the utmost tenderness. After all it was a mercyseat. If singlehanded he could not handle a patient without hurting him, let him call the other nurses to his assistance …
He would never on any account neglect to keep his mouth shut. The mercies of the Mercyseat were private and confidential.
In renaming the hospital Beckett was loudly signalling the parallels between Britain’s mental asylums and Irish institutions such as the Magdalene Homes. No one seems to have picked up the signal so perhaps it wasn’t loud enough. But for Beckett, moving backwards and forwards between Britain and Ireland in the 1930s, like half the characters in his novel, the idea that these were two different worlds was clearly nonsense. They were the same world, arbitrarily divided across two jurisdictions.
Murphy seeks a job in the hospital because he wants to test his hypothesis that a life cut off from other people is a truly free life. The ironies are obvious, given that the nurses are described as ‘sadists’, doling out physical beatings at night behind locked doors, and the therapies to which the patients are subjected are as likely to kill them as cure them. What Murphy wants to see is the view from inside the heads buried in the institution; he thinks he’ll find salvation in communion with the mentally ill. He turns out to be wrong about that. But in only seeing what he wants to see he behaves just like everybody else, including whole communities adept at turning a blind eye to their own operations, or disavowing the meaning of what they have seen.
Yes, Beegan had a message for me.
How did the ward orderlies and the nurses understand the afterlives that their patients were living in? How did my grandparents, my parents and my aunt, understand their work in the hospital? What were the stories – about the kind of suffering they witnessed, the necessity for control, the value of surgery, and also perhaps the nature of humanity – in which they had to believe to make their work bearable?
My childhood was steeped in images and stories of the hospital. The year was divided into periods defined by school and the hospital (where my mother still worked), and ‘time off’, in the holidays, when we were in Ireland. But they were two sides of the same coin. My family was formed in the shadow of these British and Irish institutions. While some people (including some members of my family) were sacrificed to the system of institutional care and banishment, others (my grandparents, my aunt, my parents and, in the end, me) became beneficiaries of the system. We were both the victims and the perpetrators. But – and this is perhaps the heart of what I am trying to get to – I suppose it mostly didn’t feel like that. It mostly just felt like life.
My mother arrived at Netherne in the spring of 1949. She was eighteen. I have a pretty clear visual image of what she was like at that time because just over a year later she appeared in a film set in the hospital. She recalled this little adventure only recently, and found herself unable to remember anything about the film except that the lead actress was blonde. I spent weeks googling actresses born in the 1920s and 1930s and checking the colour of their hair. I typed all sorts of combinations of terms into the search engine: psychiatric hospital, film, 1950s, Sheila Hancock, Netherne, asylum, depression, Sylvia Syms, and on and on until one day I was searching through the BFI catalogue and found the film free to watch online. I was so damned pleased with myself when I saw the hospital entrance appear on my laptop screen. Released in 1951, Out of True was funded by the Crown Film Unit as a public information film designed to demystify mental hospitals and get people onside with new developments in mental health care under the NHS. The blonde actress turned out to be Jane Hylton, and one of the dark-haired extras was my mother.
Out of True was England’s answer to The Snake Pit, the notorious 1948 film indicting the treatment of the mentally ill in American asylums. It’s a strange but true fact that The Snake Pit was the first film my mother ever saw, on a trip up to town with fellow nurses from Netherne. It must have come as a shock, and frankly I’m surprised she ever went back inside a cinema. ‘This is entertainment?’ Based on Mary Jane Ward’s semi-autobiographical account of her experience at Rockland State Hospital, just north of New York City, The Snake Pit starred Olivia de Havilland as Virginia, a disturbed woman who gets caught inside the nightmare of asylum care, until she is rescued by a psychoanalytically informed psychiatrist. Much of the film focuses on the series of punishing treatments Virginia suffers uncomprehendingly, including scalding baths and electric shock, and the barbaric treatment of patients considered troublesome or beyond help. A group of British psychiatric nurses, concerned that the hospitals in which they worked would be tainted with the gruesome picture of state asylums in America, tried to have the film banned in the UK. They failed, and Out of True was one consequence of their failure – an official attempt to provide an alternative and positive picture of institutional psychiatric care in Britain. And so my mother came into remote and unlikely contact with the world of Britain’s left-leaning artist intellectuals.
The Crown Film Unit had a store of radical talent to draw on. The screenplay for the film was written by the poet and communist Montagu Slater, who wrote the libretto for Peter Grimes and worked with Auden on John Grierson documentaries such as Coal Face. Elisabeth Lutyens composed the music. She supplemented her income from writing orchestral and chamber music by creating scores for horror films and her skills in melodrama came in handy, especially in the gothic opening scenes. There are sensational aspects to Out of True but they are all associated with life outside rather than inside the hospital. Jane Hylton stars as a depressed housewife, driven to the edge by – what exactly? She lives in a small flat with her husband and two children. Her mother-in-law has come to stay and the place is overcrowded; she has no time alone with her husband; she feels judged by her mother-in-law (Mary Merrall) and her nosy neighbour (Beatrice Varley); one morning she runs out of tea, and leaves the gas on by mistake. None of these is sufficient reason on its own, perhaps, to throw yourself into the Thames, and that is why she is admitted to Netherne.
She passes through the hands of various kindly and avuncular experts. She is injected with a truth drug and undergoes narco-analysis in an attempt to get to the root of the trouble. She experiences a benign and highly streamlined version of electro-convulsive therapy, administered by ultra-calm nurses in starched uniforms (the film cuts just before the current is turned on). She does art therapy and physical exercise; she befriends another patient, played by Muriel Pavlow, whose problem seems to be neurotic jealousy of her sister; and finally she has some sessions of Freudian psychotherapy with the wise Dr Bell (played by Jean Anderson). There was a real female Freudian analyst working at Netherne at the time, whose name was Dr Yates. Her film alter ego helps Jane diagnose the cause of her breakdown as an inadequate childhood relationship with her mother, which she now projects onto her mother-in-law.
The course of her treatment does not run entirely smoothly. One stormy night she gets out through the French windows of her open ward, and races through the Coulsdon woodlands to get back to her flat and her children. She is convinced that she does not need to stay in the hospital. But her reaction to the sound of a distant alarm proves that her nerves are still broken and her husband returns her to the safety of the institution on his motorbike. This escapade teaches her to trust the experts. The film has many lessons for its viewers. It is misguided to be fearful of the mentally ill. They are just like you and me, and this is especially true of neurotic women patients, and especially if you and I are women. The film also teaches that if you are one of those neurotic women it is misguided to be fearful of mental hospitals. No one gets locked up in the film, no one is a danger to anyone except themselves, and the food and accommodation are excellent.
Netherne did have a reputation for the civilised and humane treatment of its patients. It was probably not chance that the hospital was chosen as the setting for the film. In 1947 the medical superintendent at the hospital, Eric Cunningham Dax, published Modern Mental Treatment, a handbook for nurses detailing the latest therapies. The diagrams showing, for example, how to lay out instruments for administering insulin, resemble a storyboard for the shots of treatment in Out of True. The whole thing exudes clinical authority and the promise of hygienic control over mental illness. I picture my teenage mother, in a starched uniform, learning the drill. It is, in fact, very easy to picture her because I can find online a photograph of someone very like her logging insulin coma patients at Netherne in a Picture Post archive from the early 1950s. Netherne was proud of its reputation for cultivating a benign and enlightened environment in which to be ill. There were locked wards, straitjackets and padded cells, but ‘higher grade’ patients were allowed as much freedom as they could handle. In 1948 the hospital became an international showcase when Eleanor Roosevelt visited and extolled the benefits of its progressive regime, compared to the grim conditions inside state asylums in the US.
About 24 minutes into the film my mother appears. She is lying on the grass outside one of the wards reading a book. She wears a flowery dress, and behind her the Surrey hills roll out to the horizon. She is, it seems, a resident of Netherne; next to her sits another patient, flicking through a magazine. It is a scene of tranquillity, and, apparently, some affluence. In the foreground, Muriel Pavlow explains to Jane Hylton that she was at the top of her class at her girls’ school. The point appears to be that people of all backgrounds get sick, and that mental illness is no respecter of brains or bank balances. (A couple of years later, as though to prove the point, Vivien Leigh was admitted to Netherne, following a breakdown while filming Elephant Walk. Her treatment included being placed for some weeks in an insulin-induced coma, through which she was nursed by two sisters – actual sisters, Maureen and Kathleen Barrett from Galway, one of whom took the day shift, the other the night – as she lay on a mattress on the floor.)
At the end of the scene Jane and Muriel are called in to tea. As they walk back through the French windows, my mother raises her head from her book to look at them. It lasts a second, this movement of her head. I watch it again, and again, and again. I put the film on half-speed. I try to slow her movement by watching slowly, holding my breath. I am looking at my mother before I knew her, at around the age my daughter is now, moving on my laptop screen.
My mother as voluntary patient at leisure: what intrigues me about this hilltop scene is the way it points so directly to the faultline running through the new look psychiatric institutions of the 1950s. The day-to-day functioning of the hospitals, like prisons, depended on a clear differentiation between staff and inmates – those who had authority and those who were subject to it. Yet as the purpose of the hospitals shifted after the war, from being primarily custodial towards the goals of treatment and cure, they became increasingly invested in the idea that roles could change. Unlocking the wards made no sense unless you accepted that the difference between the people inside and those outside was marginal. Inmates could, and ideally should, progress sufficiently to return to civilian life (as Hylton does in the film). But by the same token the staff could regress to become inmates. The woman in the flowery dress in the background and her magazine-reading companion were not patients, they were nurses. But it would be impossible, if you didn’t already know, to tell the difference.
My mother remembers the day she was filmed as a patient. She had spent the morning as a very junior assistant in the operating theatre (passing instruments? counting swabs?) when she was asked by the sister in charge whether she wanted to be in a film. ‘Change out of your uniform quick and run across to the canteen where they are looking for extras.’ What, I wondered, went on in the operating theatre? In the early years of the hospital it was probably used for extracting the patients’ teeth, and maybe also their tonsils, testicles, ovaries, gall bladders, cervixes and parts of their colons. Surgical treatment of psychiatric disorders was fashionable in the 1920s, under the influence of the experimental work of Henry Cotton, an American psychiatrist who believed that mental illness was caused by ‘focal sepsis’, the result of untreated infections in the body.
By the early 1940s theories regarding the biological cause of mental illness had shifted attention from the organs to the brain, and the operating theatre was given over to neurosurgical interventions, leucotomies (or lobotomies) in particular. The charismatic neurosurgeon Wylie McKissock, who was based at Queen Square in London and the Atkinson Morley Hospital in Wimbledon, would turn up every six months or so and perform leucotomies on patients who had been selected by the psychiatrists. One of his junior colleagues recalled that ‘he was quite prepared to travel down to whatever the hospital was on a Saturday morning and do three or four leucotomies and then drive away again.’ My mother remembers the excitement that heralded his arrival, as nurses ran to get a glimpse of him. He motored to mental hospitals across the country and by 1957 was claiming credit for 490 surgical interventions using his new ‘rostral P’ technique (in addition to operations using the standard procedure), which he claimed took six minutes to perform. It was, he explained, ‘a very simple technique to an experienced neurosurgeon, requires no specialised apparatus or equipment and can be carried out in the simplest form of operating theatre’.
You can watch a suitably confident – almost offhand – expert explaining this technique on YouTube in a clip from the BBC series The Hurt Mind. The series ran for five episodes in the spring of 1957. In the mid 1950s almost half of all hospital beds in the UK were occupied by patients with mental health disorders, but mental illness was hardly talked about. If you were going to persuade people that psychiatry was a respectable field of medicine then something would have to be done about this stigma. The National Association of Mental Health worked with the BBC to produce a series designed, as the brief put it:
1. To allay fear.
2. To encourage the sick to take advantage of available treatment in the early stages of disease.
3. To make known the latest advances of medical science and to increase the public’s confidence in present-day medical science.
It was propaganda, though that wasn’t all it was. Watching the programmes now it seems extraordinary that anyone could have taken these doctors and their pet treatments seriously. The posh voices, the suits, the tacky diagrams of brains with arrows indicating where the incisions would be made, the box with the on-off switch for delivering electric shocks which looks like a rudimentary car battery, the nervous patients and their families prompted to give bright answers concerning their treatment (‘Oh, yes, sir, he’s just as good now as he was before’). It teeters on the edge of parody, Monty Python without the laughs. And the cracks must have been visible back then too. In the first episode, the MP and broadcaster Christopher Mayhew checks himself in to Warlingham Park Hospital (over the hill from Netherne) in order to show the audience that far from being a place of ‘hopeless misery, raving, violence, weird uncanny behaviour’, the ward, with its warm fireside, television, visiting hairdressers and morning newspapers in the lounge, is like ‘a hostel or private hotel’. Just to the other side of Netherne, however, lay Cane Hill, which Mayhew admitted was ‘ugly, oppressive, wretched … You feel you’re in a 19th-century prison or workhouse … staff shortage and overcrowding mean locked doors and gates – it’s the only way hardworking staff can manage. This gate locks patients into this exercise yard, or airing court as it’s called. It’s sunless, crowded, ugly, like a cage for wild animals.’
The point of showing the prisons and the cages was to make sense of the need for new treatments. It wasn’t until 1954 that psychotropic drugs, particularly Chlorpromazine (sold under the name Largactil) became widely available. Until then the major treatments for psychoses in Britain were insulin coma, ECT and leucotomy. If you wanted to get away from a purely custodial regime (straitjackets, padded cells, doses of paraldehyde to get people off to sleep), you had to try to prove that the new therapies worked. Individual superintendents in hospitals around the country conducted their own small-scale experiments, and Netherne’s trials are extremely well documented. Once you start looking at the studies it’s hard to know where to stop. I can read about Eric Cunningham Dax’s experiments inducing convulsions by ammonium chloride, and his opinions on the relative benefits of vertical and horizontal incisions in the frontal lobes. I can study his account of choosing fifty patients for a leucotomy trial in 1942, based pretty much on how much of a nuisance they were. ‘They formed a large proportion of the most violent, hostile, noisy, excited, destructive or obscene cases in the hospital; the type who distress their relatives, upset the other patients and consume the time and energy which could be put to so much better purpose by the staff.’ I think of the ward where J.J. Beegan spent those years. Two of the patients in the trial died, but apparently the others became more docile.
I can discover that insulin therapy was the speciality of R.K. Freudenberg in Berlin (until he fled in 1935) and then in Vienna (until he fled in 1937), and that he eventually brought his expertise to Netherne. And I can watch this treatment being carried out by nurses at Netherne in the third episode of The Hurt Mind. No one mentions the mortality rate, and the fact that there was no proof at all that it worked. I can learn of Freudenberg’s growing disillusion with physical therapies, of the pioneering studies done at Netherne into ‘industrial therapy’ for long-stay patients, and the pilot schemes to determine whether a small-scale therapeutic community could be created within a large asylum. In 1957 Freudenberg went on a course for medical superintendents where he worked with some of Britain’s most innovative advocates of therapeutic communities and open doors: Maxwell Jones, Duncan Macmillan, David Clark. And he brought some of that excitement back to the hospital with him. By the mid 1950s there was a resident sociologist at Netherne, producing studies of social behaviour inside the hospital. Then there is all the material on the work of Edward Adamson, the art therapist, and the huge collection of his patients’ artwork. The hospital is a historian’s dream, it is so well documented. The prize, surely, is that Netherne is described as Hospital A (the ‘best’ hospital) in a major study of ‘institutionalism and schizophrenia’ that lasted through most of the 1960s. There are whole books in which Netherne features as a central character. I read all of this in the hope of better understanding the way people thought about hospitals and treatment fifty or sixty years ago. But all I really got from it was a sense of the speed at which they changed their minds.
I searched the anonymised case histories for a detail that would tell me what it felt like to be a subject of these studies and experiments. The patients flitted like ghosts across the pages. To my embarrassment, I couldn’t rid myself of a mental image of animals glimpsed in the wild – the odd sightings of the patients in these official studies are like flashes of life in an alien habitat. But the metaphor seems obscene given that these patients were (or had been) pretty much imprisoned. A zoo, or a circus, might be more apt. They were being observed and recorded and logged to an excessive degree, yet their inner lives seem impossible to capture. Georgia N., for example, who was part of a large-scale study of the rehabilitation of schizophrenic patients in the early 1960s. She ‘was admitted for a few months during 1949, when she had a leucotomy, and then again in 1950 when she was aged 39. It was said that she had a “persecution complex”, heard remarks in “the other seven languages” and had been ill at least since 1943.’ In 1964 she was much the same but ‘her appearance was still smart and attractive’. Or Dorothy Q., who was admitted in 1952 at the age of forty, when she was described as ‘domineering, cantankerous and argumentative. She complained vaguely of various somatic influences and lived on bread and tea in order to control them. She was untidy and withdrawn and thought that everyone in the neighbourhood was against her.’ Twelve years later ‘she still made many complaints and was extremely suspicious about every question asked. There was pressure of talk with very little content.’ These women were clearly ill as well as cantankerous, but it’s hard to imagine that subjecting them to rigid classifications and quantitative research tools (behavioural indexes and social withdrawal scores) was going to make them any better.
One of the trials at Netherne involved getting patients to fold boxes for four hours a day, four days a week. ‘Two indices of output were used – Initial Output, the number of boxes completed during the first full one-hour trial; and Peak Output, the greatest number of boxes completed during any one-hour trial.’ The winner was ‘a paranoid schizophrenic with marked, coherently expressed delusions’, who folded six hundred boxes in his first hour, and 1700 in his fifteenth. It was a well-meaning trial, part of a study using numerous other ‘indices’ that was designed to find out which kinds of patient were most likely to succeed outside the hospital. But its authors didn’t discover much they didn’t already know. And in the end it was drugs, not box-folding, that made the difference to the long-stay patients, and eventually resulted in the closure of these institutions in favour of day hospitals and community care.
In the late 1960s, after settling us all at school, my mother returned to work at Netherne with these new tools to hand. She was in the vanguard of community care provision, which meant, in her case, a great deal of driving across Surrey to visit patients in their homes and administer drugs. She also talked to them, but what I remember was the square black briefcase with a small key, containing little vials and needles. We had biros at home printed with the names of various drugs, and notepads splashed with advertising slogans like ‘Largactil, For All Your Mental Health Needs’. There was talk at the supper table of ‘pressure of speech’ (it was years before I understood this to be a symptom of mania; I assumed it meant someone with a lot to say), lithium poisoning and delusional states.
My younger sister and I would go with her on nursing visits after school or in the holidays. Sometimes we got to wait in the back of the car, reading comics or rolling about and fighting in the back seat. Sometimes we went inside. I remember the stench of urine that hit you at some of the front doors; the tottery bodies and displaced-looking faces; the abandoned kitchens, ancient bottles of orange squash and stale rich tea biscuits; the fear of being spoken to and not knowing what to say. But the home visits were vastly preferable to the days we spent at Netherne itself, patrolling the corridors while waiting for the clinics she worked in with Dr Freudenberg or Dr Forrest to end. It may be that my recollection of the corridors and their looming-largeness is a false memory. I cannot actually have spent much time in them, except when getting from one room to another, or visiting the lavatory. But at the age of eight or nine I was petrified by the unknown world of the patients, and by the horror of what I would find if I opened the wrong door by mistake.
The history of postwar British psychiatric care, from locked wards and psycho-surgery to psychotherapy in the community, can be tracked with remarkable precision through my mother’s working life. She learned to nurse patients placed in induced comas; she assisted the surgeon during brain surgery; she poured medicine down the throats of patients being held down against their will; she prepared patients for electro-convulsive therapy, and brought them round again afterwards. She learned the uses of the new psycho-pharmacological drugs and how to administer them. She was one of the first nurses to be trained for work in the community. Shortly before she retired she was working as an NHS psychotherapist. Although part of me is fascinated by this cleaving together of an individual life story and the chronicle of an institution, I am also slightly alarmed by it. Didn’t she question any of it? I understand that each type of treatment must have seemed convincing at the time – until it was passed over for the next. I understand that this is the way historical change happens. The past has to have been believed in by a sufficient number of people to qualify as the past. But it bothers me that she was so docile. I am troubled by the thought that she could hold on so tightly to the narrative of the institution even in its most punitive and brutal guises. I am uncomfortable with the idea that her worldview, and perhaps also her view of human nature, were in part constituted by the regime.
It seems unremarkable to say that everyday life on a small family farm in Ireland and life inside a modern, bureaucratic organisation were worlds apart. I can play the oppositions: the small farm and the big city; the local community and the impersonal institution; the known and the unknown. But I am not sure that any of it gets me very far, because I am left with the basic question: why did my mother and the thousands of other Irish girls who worked in the institutions fit in so well? Why did they feel so at home? Was it because, despite appearances, that world was not alien to them at all, but familiar?
One of the words used at the supper table was ‘institution’, but only in its adjectival form. The problem with this or that patient was that they had become ‘institutionalised’. When my older sisters complained about particularly annoying or rule-stickler nuns at their convent school my mother laughed and said their problem was that they were institutionalised. (I was spared the convent, by not performing well enough in the entrance exam. This was a source of disappointment to my parents, but even then I knew it was a lucky break.) On the shelf at home was the Pelican edition of R.D. Laing’s The Divided Self. I remember it because it stuck out a bit beside the Edwardian set of the novels of Charles Dickens, picked up at a jumble sale or second-hand shop, and the books we actually read, stories by Rosemary Sutcliff, Alan Garner and Agatha Christie. When my eldest sister went to Birmingham University to study English in the mid 1970s the bookshelf began to change character: T.S. Eliot, Camus, the Mabinogion. It may be that Laing was part of Birmingham’s contribution to the family’s store of knowledge. But I think it’s more likely that my parents bought it in the 1960s, when debates about madness and institutions were highly charged.
From the early 1940s there was talk of the dangers of institutionalisation, of opening up the wards and ending the stigma against mental illness. The superintendent at Warlingham Park (the hospital Christopher Mayhew likened to a private hotel) had begun unlocking and ‘humanising’ his wards as early as 1935. And at the end of the war there was a steady stream of calls for an end to closed institutions. One of the most influential studies in Britain was by Russell Barton, whose book Institutional Neurosis (1959) argued that a set of debilitating symptoms, including apathy, submissiveness, lack of expressiveness and loss of interest, was caused by the regime in the hospitals themselves. Barton, who had volunteered as a medical student to join the relief of Belsen, wasn’t the only person to draw comparisons between NHS psychiatric hospitals and concentration camps. By the early 1960s a huge range of scholars and practitioners were lined up against the asylums, from the anti-psychiatrists Laing, David Cooper, Jean Oury, Félix Guattari and Thomas Szasz, to Michel Foucault and Erving Goffman. The major studies of asylum culture by Szasz, Foucault and Goffman were all published in 1961. It was a zeitgeist, and it soon changed the way institutions were thought about inside the institutions themselves. And from there the way they were thought about around our supper table.
It isn’t so long ago that I first read Goffman’s study of asylums as ‘total institutions’, but when I did I recognised that his ideas silently framed my childhood. The four essays in the book were first published in the late 1950s, and their impact at Netherne was almost immediate. Within a year Rudolph Freudenberg had started a ‘resettlement unit’ designed to break the hold of the ‘total institution’ on patients, and teach them the skills they would need once they had returned to work and live in the community. It was the hospital’s brave new world, and it was where my mother got her first job when she returned to work after we started school.
Goffman was a Canadian sociologist who did his first research on Shetland in the early 1950s, looking at ‘the presentation of self’ in everyday interactions between islanders. For Asylums he spent a year doing fieldwork at St Elizabeth’s, a hospital in Washington DC with seven thousand inmates. His book reflected a broad consensus among sociologists and social anthropologists on life inside the postwar asylums, as well as prisons, convents, army barracks and concentration camps. There is evidence of institutional brutality and neglect in Goffman’s book, particularly when he turns his attention to the punishment and rewards of the ‘ward system’. He corroborated the existence of the organised scheme of ‘levels’ revealed in The Snake Pit. He was scathing about the forms of dispossession to which inmates were subjected in order to encourage them to submit to social control – removal of their personal possessions and sometimes their clothes, and (in extreme religious institutions and penitentiaries) their names and even their ages. He acknowledged that many of the hospitals were ‘storage dumps for inmates’, designed to protect the wider community from pollution, but that they had to be presented to the public as rational organisations designed to produce results in the form of alleviation and cure. But what Goffman was most interested in was the stories people had to tell themselves in order to believe in the institutions, and the language they used to tell them.
Aware that there were many sick people who hadn’t been committed to asylums, as well as many not very sick people who had, Goffman argued that ‘mental patients distinctively suffer not from mental illness, but from contingencies.’ Contingent circumstances – how far you lived from a hospital, how willing your relatives were to care for you, how much money they had to share the burden, whether there was someone at home willing to take you back – made the difference between becoming a patient and not becoming one. But the more arbitrary the circumstances that led you to the institution, the more your committal had to be represented in terms of necessity. What he called the ‘moral career’ of the mental patient involved adjusting to the narrative in which it was reasonable, indeed beneficial, for them to be deprived of freedom, relationships and rights, and to be subjected to communal living, arbitrary authority and the violence of various treatments. Accepting the necessity of your incarceration in an institution was known as ‘settling down’; it entailed ceasing to struggle against the reality of your situation. But what Goffman stressed was that this involved more than simply adjusting to the demands of the ward system and learning to accommodate oneself to a regime of rewards and punishments – it required a whole new understanding of the self, in effect a new life story.
Take the patient’s case history. Like all life stories the case history was constructed retrospectively. The moment a patient entered the asylum what had felt like ‘life’ was recast as a set of symptoms and clues to an underlying illness. The case history gathered together the information that pointed to the diagnosis that explained the fact of being a patient. It was a closed circle. And since what was at stake for the patients was nothing less than the nature of their human nature, whatever happened to them was expressive of their whole self – so that through the unfolding case history a patient’s past mistakes and present progress were under constant review. The paradox, for Goffman, was that the emphasis on moral or ‘human’ progress resulted so often in a kind of fatigue. One of the best ways to survive the ups and downs of the asylum’s rigorous but arbitrary moral climate was to cultivate a kind of ‘civic apathy’. It was far easier to be resigned to your fate as a hopeless case than to strive against it. In other words, you might as well just give up. The process Goffman was describing was one of learning to consent. As patients consented to their own condition as patients they were helping the staff to make the institutions work.
Goffman had less to say about the moral career of the staff, whose job it was to steer the patients along the hospital assembly line, with all the bureaucratic documentation and paraphernalia this entailed. That the staff had a good deal to gain from consenting to play their part is obvious: there was security, wages, training, sometimes a home, and sometimes a career to be had. Goffman argued that the contradiction between what the institutions did, and what their officials said they did, formed the basic context of the staff’s daily activity. Whether the primary aim was custody or psychiatric care of patients, the moral climate in which patient behaviour was measured provided a key to meaning for both patients and staff. ‘Industrial’ or work therapy, for example, on the farm, the bakery, the laundry or the wards, was mostly without pay. The meaning of work was redefined so that it was now a matter of enhancing the patient’s moral and human capacity. Put crudely, the institutions required that patients learned to articulate their capacity to be human, and the staff got paid for constructing the framework that allowed that capacity to be expressed.
I am fascinated by a passage in Goffman’s book where he describes a play put on by the ‘higher grade’ patients at St Elizabeth’s for the benefit of local fundraisers and philanthropists. It was a version of my mother’s shift from nurse to ‘good’ voluntary patient in Out of True, but this performance involved ‘good’ psychiatric patients playing ‘bad’ versions of themselves:
I have seen mental patients from good wards give a well-advertised, public stage performance of conditions which presumably used to prevail in backward mental hospitals. Victorian costumes were used. The audience consisted of psychiatrically enlightened well-wishers from the environing city. A few buildings away from where the audience sat, equally bad conditions could be observed in the flesh. In some cases, the performers knew their roles so well because they had played them.
These patients were involved in propaganda at their own expense – a pretence that workhouse conditions had been left behind with Victorian costumes. In fact Goffman was arguing that the whole structure of institutional care was built on performance. Whether the focus was on custody (cages), or treatment (warm firesides), the asylum framework required people to play the roles allotted to them. The institutions would cease to work if patients refused to consent to their role as patient, and the staff questioned their role as staff.
My mother’s nursing career was a successful story of healthy progress that depended on an opposing story of illness. Goffman would have been delighted with the way she could appear to swap roles simply by changing out of her uniform and into a summer dress, since it pointed to the fact that, deep down, the differences between staff and patients were theatrical, not material. And in fact the slippage between roles was continually played within the institutions themselves. The Christmas pantomimes, the hospital newspaper, the sports events, the open wards and patient visits to the local village were all ways of demonstrating the basic similarity of the players. But the bureaucratic workings of the institution depended on everyone playing their role as though they meant it. In One Flew Over the Cuckoo’s Nest Randle McMurphy feigns mental illness because he thinks that incarceration in a mental institution will be a softer option than prison, but he ends up being trapped – and destroyed – by the role, because he refuses to consent to it.
But I don’t have to go to American films to find a story about swapping roles. There is one far closer to home, about my mother’s friend Gibson. I have known this story since I was nineteen or twenty, and away at university for the first time. Gibson was my mother’s best friend – an English girl from the West Country who trained alongside her at Netherne. They were not the most likely duo: Gibson, I think, was from a relatively well-off background, an only child, her father a civil servant. She had worked as a commercial artist for a few years after the war, until she decided she wanted to train as a nurse. It was an odd choice, when you think about it. Nursing was low-grade work, a job for immigrants, from Wales, or Ireland, or later from the West Indies. Nonetheless Gibson chose it as a career and she and my mother became inseparable. When my mother left Netherne and went to Mile End Hospital for general training she wrote to Gibson and suggested she join her, which she did. When she moved on again to Whipps Cross Hospital, Gibson went too. For four or five years, in three different hospitals, they were a team. I know about these friendships – the ones you have when you first leave home to make your way on your own. They are part of the fabric of learning who you are, or who you could be, and they last for life, or they can do. But not in this case.
My mother hadn’t seen Gibson since before I was born, though she still told stories about her, which were usually very funny, like the jokes they had at the expense of their pompous lecturers, several of whom had been discharged from the army and still gave themselves military airs. But there always appeared to be a kind of hesitation, a catch in the throat, that hovered around Gibson’s name. I can’t remember if I ever asked if they had fallen out, or why, but one day my mother blurted it out. Sometime in the late 1950s, after my parents had married and moved away, Gibson had asked for, and been given, a leucotomy. I still remember my feeling of horror, of disbelief, on hearing this story. She had wanted to relieve her anxiety, my mother said. She had wanted to release herself from the burden of her thoughts. I was incredulous. To volunteer to have your brain cut? To trust someone like the offhand doctor who juggled a plastic brain on The Hurt Mind? To believe in it that much?
I pressed on wildly, asking for more. I wanted to break through the barrier of things not said, and looking back now I feel both sympathetic to my younger self – impatient of politeness, hungry to understand – and ashamed of her. Why did I think I had the right to know? I saw my mother’s sadness, but it didn’t stop me.
‘I think,’ my mother said eventually, ‘she was unhappy about her sexuality.’ I stared at her. At least I knew to stop asking. And it had all been said anyway. A few years after the surgery, my mother said, Gibson killed herself. It’s funny what you ask about and what you don’t. I didn’t ask why – it seemed obvious. And I didn’t ask how; it seemed cruel.
I didn’t ask, and it feels strange telling the story now. The trouble with recounting Gibson’s story is that I’ve approached her as though she were a case history. She appears here as proof of something, in the same way as Georgia N. or Dorothy Q. in the Netherne studies. Or at any rate not in a different enough way. I have too little to go on to get close to Gibson as a person, but I’m loading meaning onto the bare bones of what I know, nonetheless. I feel uncomfortable, but the more uncomfortable thought is that Gibson may have thought about herself as a case history too. She tried diagnosis and violent intervention for an affliction for which the cure should have been love. She trusted in the hype surrounding the new physical treatments. She believed in it all too much, and perhaps she needed to. She gave her consent even when it wasn’t asked.
What I caught in my childhood visits to Netherne at the beginning of the 1970s was the tail end of a period in which these hospitals functioned primarily as places of confinement. They were beginning to be dismantled in favour of community care, and the fact that my sister and I could wander about in the corridors was one sign of the more open therapeutic environment that was coming into being. Netherne was progressive and it must have felt good to be part of that experimental wave, especially given the grim reputation of psychiatric care in Ireland. Ireland had the highest proportion of the population in psychiatric institutions in the world, and the patients there were the least visited. The boundary between the inside and the outside of the institutions was not only more porous in England, but – as the survival of the Irish Mother and Baby Homes and the huge asylums indicates – the difference was growing. For my mother, moving to England in the late 1940s meant moving to the future.
Instrumental to that future was a change in the nature of consent to the system. In the total institutions described by Goffman, the patients’ consent to their condition as patients differed little from acquiescence. And a kind of silent acquiescence was also required from people who lived on the outside, people who knew the institutions existed (and perhaps had family members inside) but preferred not to know too much about what went on in them. This was a model in which the institutions were wholly imbricated in the workings of the community, but at the same time wholly cut off – invisible to ordinary sight. A friend of mine from Dublin likes to play a kind of parlour game in which he asks locals to tell him the location of Grangegorman, the huge Dublin psychiatric hospital that was decommissioned in 2013. It’s on the north side, centrally located between Phoenix Park and O’Connell Street, and is now part of Technological University Dublin. But everyone puts it out in the country somewhere, or they guess at suburbs such as Artane or Santry or Ballymun. The hospital was and is an almost mythical building, both there and not there, looming large but impossible to locate.
When the doors of the hospitals were opened – to film crews, politicians, Picture Post journalists and small children – the boundaries between the civilian world and the world of the inmate were blurred. This was a process driven by changing conceptions of mental health as well as, crucially, the use of psycho-pharmacological drugs. The community that had to consent to the way the hospitals worked extended to the public at large. A different kind of legitimacy was being sought. The narrative of the progressive institution disarmed critique and solicited public affirmation and consent. But with the suggestion that we were all potential patients the boundaries of the hospital became hard to discern. Technically there could be no inside or outside to the institution, and people like my mother’s friend Gibson could consent to their own damage without passing through any doors.
In 1971 another film was made at Netherne by a government-funded organisation – this time the Arts Council. It is a portrait of the sculptor Rolanda Polonsky. Netherne’s reputation as an enlightened institution was enhanced by its pioneering role as a centre of art therapy under Adamson’s leadership. In 1946 Eric Cunningham Dax invited Adamson to set up an art therapy studio in the grounds, and this was later expanded to include an exhibition space. Initially the art rooms were a form of research laboratory. Each patient was given the same size of paper, identical easels and the same pencils and paints so that their products could be compared scientifically. This was where J.J. Beegan covered his sheets of paper with ‘esoteric writing’. The patients’ art was regarded as additional ‘evidence’ to be added to their case history. Eleanor Roosevelt lamented the fact that during her visit to the hospital in the spring of 1948 she hadn’t had time to visit the art studio:
I was sorry I did not have a chance to look at a book of paintings done by patients. Many of them have never painted before, and to a psychiatrist I’m sure these paintings would tell volumes about the mental condition of a patient in different stages of his illness. None of them receives instruction. They just paint what they have in their minds and want to put on paper.
The psychiatrists, too, thought they could tell volumes. Cunningham Dax’s colleague Francis Reitman, director of clinical research at the hospital and a strong believer in the theory that mental illnesses had organic causes and therefore could be cured by physical treatments, was keen to use the studio as a way of testing visual expression before and after leucotomy. Netherne was his laboratory, the patients were his guinea pigs, and like everyone else at the hospital he published his findings, in his case in a book called Psychotic Art which came out in 1950.
Adamson was certainly less dogmatic than his superiors. He was interested in Jungian ideas about creativity and he broadened the remit of the studio such that, over his 35 years at the hospital, it became less and less associated with research, and more and more a place of artistic experiment and self-expression. Yet Adamson’s recollections of his first years in the hospital, in the late 1940s, remind us that for all the ‘front of house’ show put on for outsiders, Netherne too had its punishing ‘back’ wards and systemic structures of neglect and dispossession. On his first visit in 1946 he had passed ‘through long corridors and many locked and relocked doors’, to discover the large hall where Beegan was sheltering along with a hundred others ‘swathed in bandages’ and ‘disfigured by post-operative bruises and black eyes’. This was the ‘deteriorated’ ward and these were the patients on whom Cunningham Dax was experimenting with leucotomies. Adamson saw some of that violence and suffering reproduced in the art studio, and because he collected much of the work that was sanctioned there, and encouraged the Arts Council to make a film in the 1970s, we can see it too.
We do not know if J.J. Beegan ‘sculpturer’ was trained as an artist before he was committed to Netherne. But we do know that Rolanda Polonsky had gone to art school and that some of her pieces had been exhibited in small shows. Her work was not naive, untutored self-expression (‘They just paint what they have in their minds’), the kind sought by doctors such as Reitman, and – for different reasons – by the Art Brut movement. Polonsky was born into an upper-middle-class family in Northern Italy in 1923. Her parents were both opera singers and her maternal grandfather was the English writer and philosopher Thomas Bailey Saunders (an authority on Schopenhauer). In 1947 she graduated from the University of Florence with a degree in political science. She travelled to Paris in connection with a commission, and studied for a short time, probably informally, at the Académie de la Grande Chaumière.
It’s unclear why she came to Britain. Perhaps she came to visit relatives; perhaps she came on one of the immigrant work schemes that were available to young Italian, German and Baltic women looking for an escape from the extreme poverty of postwar continental Europe, although this seems unlikely given her background. Perhaps she travelled in connection with a small exhibition of her sculptures that was held at the London Gallery in 1950, organised by the Belgian Surrealist poet and painter E.L.T. Mesens. It’s possible that Mesens encountered Polonsky’s work in Paris after the war, but it seems more likely that Adamson arranged for it to be exhibited in London. He knew Mesens and the owner of the London Gallery, Roland Penrose, and collaborated on a later exhibition of ‘schizophrenic art’ at the Institute of Contemporary Arts. And by the time of the London Gallery show, as the catalogue notes coyly, Polonsky was ‘living and working in England’. At some point in the late 1940s she appears to have suffered an acute psychotic episode. She must have been admitted to Netherne soon after she arrived in England, because by the time the Arts Council film was made in 1971 she had, according to the commentary, been in the hospital for 24 years. When Roosevelt visited in 1948 she was probably scrubbing floors in the wards, which is what she was doing when Adamson found her.
But the Arts Council wasn’t interested in her history. The ten-minute film, directed by the artist Lionel Miskin, wants its viewers to think about what can be learned from looking at art made without the expectation of its being seen by an audience. It wasn’t only the meaning of work that was redefined by the institution, but the meaning of self-expression. The voiceover explains that Polonsky is schizophrenic. ‘Her illness which has caused her such affliction has in fact tapped a deep source of mystical vision and human feeling.’ There is something distinctly voyeuristic about the way in which viewers are encouraged to consider this vision as the product of not only a sick, but an imprisoned mind: ‘In the supposedly sane world of society the artist enjoys an expectancy of family life and friendship and some degree of acknowledgment for the work produced. The artist is perhaps more conscious of our surrounding environment than most people. By contrast the schizophrenic paints or sculpts in the confined world of the mental hospital.’
Polonsky herself is a fragile figure. She walks with hesitation through the hospital corridors (they bring me back to my eight-year-old self); she talks softly in halting English and her eyes blink against the light. Her subject matter is Christian iconography, and what she calls ‘the eternities’. There are repeated images of the cross, the deposition of Christ, hands supplicating in prayer, angels, multitudes. As she glosses each work of art for the camera it becomes clear that every detail has a meaning for her, and a correspondence. Polonsky is not interested in the aesthetic appeal of her art – she says nothing about form or style. The idea of an audience outside herself seems unfamiliar and unimportant to her. Instead the paintings and sculptures are a way of thinking about and making sense of pain. She reaches for Christ’s suffering on the cross as a way of understanding – or giving meaning to – her own suffering.
Several of the pieces she glosses for the Arts Council film were plaster maquettes for a series of the Stations of the Cross, planned as a set of fourteen reliefs and an altarpiece for the Netherne chapel. They are now held in a store at the Bethlem Royal Hospital in Beckenham (Beckett’s Magdalen Mental Mercyseat). When I went there recently to see them I was amazed at the contrast between the size of the pieces (some of them are ten feet across) and their handmade quality. The reliefs have been created without tools – you can see the finger marks where Polonsky kneaded the plaster into the shape of a suffering Christ, or a penitent crowd of people. I could fit my fingers to her finger marks. It is as though her body, the weight of her fingers and the pressure of her hands, still lingers in the plaster. The reliefs are like emanations of a body that seems far more solid than the uncertain person speaking in the film.
As she points out to the camera the penitent, suffering bodies she has made, Polonsky says ‘This is simple’ or ‘This is very simple.’ ‘This is the calculation of the last supper,’ she says, of a drawing of a strung-up and strangely impaled body. The spidery figure, drawn without lifting the pencil from the paper, is like a diagram of torture, with dark circles for breasts. She explains that her vision of the body on the cross is ‘not being a man but woman. Because, on my modest opinion, it’s the woman that has more crosses in the world than the man itself.’ She describes a series of pencil-drawn bodies in grotesque and tortured poses, hanging as though by their necks, as ‘the Last Judgment done not by paradise but by the damned. Because at the last morning as the prophet has told us, also the damned will speak and have to say their word.’
She stands with her head tilted back, mirroring the pose of a thrown-back, sculpted head of a girl. This, she explains, is a representation of
a girl who has lost her virginity. So, she’s so surprised by the sensual act of man, that she doesn’t know what to think, or what to do. She’s hell and heaven in this moment, thinking back of her old life of the first years and you are an innocent. And suddenly she’s grown up, and that is this portrait, of this moment.
The scene is hard to watch. If this isn’t personal experience it is certainly extreme identification. There are further representations of female bodies, mothers with infants, and many, many bodies in pain: ‘I think that all people are broken, in all life. Life passes, but the people are broken just the same. And so, I represent it with Jesus. Jesus there is broken, and his life has been taken away, because … because he’s pushed aside.’
Polonsky’s story has been constructed entirely inside the institution where she has had to learn – in English – to accommodate herself to a life pushed aside. She has resigned herself, and she turns to religious iconography in order to give shape to that resignation. The small vocabulary, mostly learned, I imagine, in the hospital, echoes her circumscribed life within the institution. It is a form of speech that keeps circling back, through repetition, to a primal hurt she cannot express. Something here is unspeakable, and it is hard to ignore the possibility (perhaps one should say the likelihood) that Polonsky’s life was broken by sexual violence. She was unmarried when she entered the institution and remained so. The girl was ‘so surprised’, she tells us, gently. She didn’t know what to think. Her sculptures – and the way she glosses them – force us to speculate that her own experience of having her life ‘taken away’, and of being incarcerated for (in the end) more than 35 years, was particular to the crosses women have to bear.
I imagine other stories for her. Apart from leucotomy, the simple operating theatre at Netherne was also used for terminations, or what were known before the passing of the 1967 Abortion Act as therapeutic abortions. Abortion was legal in cases where the mother’s life was in danger, and psychiatrists could recommend it for women suffering psychosis and depression, and for women threatening suicide, very often single women. In the first couple of years after she arrived at the hospital in 1949 my mother estimates that she was present in theatre for perhaps six of these surgical interventions. She was, in effect, helping to officiate in one of the secular alternatives to the Irish Mother and Baby Homes. Do Polonsky’s repeated images of mothers and babies speak of what she has lost? ‘The people are always with an infant,’ she says in the film. ‘You don’t see people without an infant, because the infant is life.’
In imagining a past for Polonsky I am, I know, fighting against her own representation of her life, which was timeless – an expression of ‘the eternities’. It was a story of correspondence and metaphor, rather than a story with a past and a future. Those had, after all, been taken away from her. She had lost contact with her past before she entered the hospital and she seemed to accept that her future was more of the present. In fact, Polonsky was eventually rescued by her sister, who came on a visit from Paris and was, in effect, shamed by a doctor who asked her: ‘Why do you leave your sister in this place?’ Polonsky chose to live the last years of her life in a convent in her home town of Rovereto. She chose another institution. But in 1971 she had settled down to her half-life existence, and the story she told was about meaning rather than experience – in fact all personal experience had been emptied out of it. She had erased herself.
I am haunted by the figure of Rolanda Polonsky, walking through those hospital corridors. If my eight-year-old self had opened the doors that frightened me I might have found her, back then, exactly as she is now in the film I watch on my laptop. And it appears to me now that that’s why I was fearful: I didn’t want to hear the message she had for me. But she hovers like an uninvited guest from a half-remembered past – and she will not go away. What is it that she wants me to see that I do not want to see? What is it that she wants me to know?
The ‘moral careers’ of Rolanda Polonsky and my mother were parallel to each other, and indeed dependent on each other. They both arrived at the hospital around the same time, and they both spent most of their adult lives inhabiting, and inhabited by, the institution. We were all walking those same corridors in the 1970s, but some of us came from the outside, and some were locked in. Polonsky was clearly ill, or had been, but by the 1970s part of her affliction was the hospital itself. Art was her means of expressing her suffering, but presented for the Arts Council cameras it also formed part of the official narrative of the institution. Art therapy stories were a way of validating the consent given by the public to the institutions as a whole. I was brought up inside that model of affirmation. The stories that my grandparents and my parents told of the institution were of productive lives – careers, marriages, families and futures were all built on working at Netherne. They were stories that fitted the progressive narrative of the institutions, dedicated to treatment and cure, until they were dismantled in favour of another model, of care in the community. And they are not untrue stories. They are, however, incomplete.
For a long time I thought that Polonsky’s story haunted me because it stood for the absolute alternative, the negative, to my mother’s story, and that is, of course, largely true. They were women of a similar age who arrived in Britain in the years after the war and while one of them was able to make a success out of her association with the hospital, the other (though she found a way of living) remained subject to it. While my mother might have played at being a patient, she never had to experience the reality. Yet I wonder if there isn’t a further message I am unwilling to hear – that the two women’s stories were aligned. Both women, as emigrants, were separated from a past at home that carried on without them and from the futures they might have had there. Both contributed to the story of psychiatric advancement. But at the core of Polonsky’s art lay a truth that went against this story of progress: despite the sunlit grounds and the airy wards and the seemingly porous border between the inside and the outside of the institution, you could still be buried alive there.
Listen to Clair Wills discuss this piece with Thomas Jones on the LRB Podcast.
Send Letters To:
The Editor
London Review of Books,
28 Little Russell Street
London, WC1A 2HN
letters@lrb.co.uk
Please include name, address, and a telephone number.