Rise of the Superbugs
Hugh Pennington
In 2014 the prime minister commissioned Jim O’Neill to conduct a review and make recommendations to ‘defeat the rising threat of superbugs’. O’Neill’s final report, published on 19 May, predicted that superbugs could kill 10 million people a year by 2050, the equivalent of one person every three seconds, more than cancer, with a cumulative cost of around $100 trillion.
Its recommendations are unarguable: a massive global awareness campaign; improving measures to prevent infection; better surveillance of drug resistance; better use of antibiotics, including the elimination of unnecessary use in agriculture; incentives to promote new antimicrobial drug development. And as an economist O’Neill can escape any suspicion of pandering to self-interest when he recommends better rewards for healthcare workers in the field of infectious diseases and for scientists studying the microbes that cause them.
O’Neill says that ‘negative externalities’ contribute to the market failure that drives antimicrobial resistance (AMR). ‘Externality’ is economist’s jargon for the cost or benefit to a third party of a decision over which they have no control. Alexander Fleming used the externality argument in his 1945 Nobel Lecture:
The time may come when penicillin can be bought by anyone in the shops. Then there is the danger that the ignorant man may easily underdose himself and by exposing his microbes to non-lethal quantities of the drug make them resistant. Here is a hypothetical illustration. Mr X has a sore throat. He buys some penicillin and gives himself, not enough to kill the streptococci but enough to educate them to resist penicillin. He then infects his wife. Mrs X gets pneumonia and is treated with penicillin. As the streptococci are now resistant to penicillin the treatment fails. Mrs X dies. Who is primarily responsible for Mrs X’s death? Why Mr X whose negligent use of penicillin changed the nature of the microbe.
AMR was a problem before penicillin. Sulphonamides were used to treat gonorrhoea from 1937. But ever-increasing doses were needed for success. Penicillin came just in time to stop a reversion to urethral irrigation with antiseptics. In the early days supplies were limited. In 1943 gonorrhoea was causing more harm to British soldiers in North Africa than the enemy was. But what about the wounded? Churchill was sent a memo raising the question. His marginal comment in green ink settled the matter: ‘This valuable drug must on no account be wasted. It must be used to the best military advantage.’ The wounded had to wait.
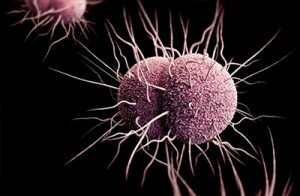
Neisseria gonorrhoeae, the cause of gonorrhoea, typifies the AMR problem. Over the last 70 years, strains developed resistance first to sulphonamides, then penicillin, then tetracycline, then ciprofloxacin, then cefixime – and we hope that it won’t develop resistance to the last ditch drugs, ceftriaxone and azithromycin. The only good news for people with multiple sex partners and an aversion to condoms is that Treponema pallidum, the cause of syphilis, is as sensitive to penicillin as it was in the 1940s. Its specialised genome lacks the genes that could code for resistance mechanisms. But it is unique among microbes in that regard.
I enjoyed pathology at medical school. In my penultimate year, 1961, I bought Recent Advances in Clinical Pathology. Its first article was ‘Source and Control of Antibiotic-Resistant Staphylococcal Infection in Hospitals’ by Mary Barber. In it she describes nearly all the medical measures to combat AMR that are in O’Neill’s report. One remedy missing was the development of new antibiotics. Barber was pessimistic:
Penicillin was followed by the discovery of streptomycin in 1944, chloramphenicol in 1947, aureomycin in 1948, erythromycin in 1952, novobiocin in 1955. But as each new antibiotic was introduced, strains of staphylococci resistant to it began to make their appearance.
Another drug came out just after her article was published: methicillin, the M in MRSA. Barber’s hopes from political initiatives were high. Her bacteriological influence was strong. But she died in a car crash in 1965 on her way to a CND meeting. Let’s hope O’Neill has more international success than that organisation did.
Read more in the London Review of Books
Hugh Pennington: MRSA · 15 December 2005
Comments
I'd just add that the prospect of getting regulations into daily practice is almost impossible. In fact, the prospect of simply regulating big biz agriculture, in the USA especially, is today impossible. The agency in charge--USDA--thanks to Republicans {and possibly Trump) in Congress, gets away with anything they like, including massive applications of glyphosate on alfalfa and human food crops.